Current Issue
A Rare Case of Acute Mesenteric Ischemia Associated with Multiple Intestinal Perforations
Krishna Kumar*, Moorat Singh Yadav
General Surgeon, Department of General Surgery, All India Institute of Medical Sciences, Bhopal, India
*Corresponding author: Dr. Krishna Kumar, General Surgeon, Department of General Surgery, All India Institute of Medical Sciences, Bhopal, India, Tel: +91 9479824972, E-mail: [email protected]
Received Date: July 15, 2024
Publication Date: September 11, 2024
Citation: Kumar K, et al. (2024). A Rare Case of Acute Mesenteric Ischemia Associated with Multiple Intestinal Perforations. Surgeries. 4(1):11.
Copyright: Kumar K, et al. © (2024).
ABSTRACT
Introduction: Acute Mesenteric Ischemia is an uncommon surgical emergency with significant mortality caused by the reduced blood supply to the intestines, which leads to inflammation and necrosis of the gut. Due to its rapid progression and association with high mortality, it causes significant challenges in the diagnosis and management of the disease. Case Presentation: This is a case of a 53-year-old male brought to emergency with complaints of bilious discharge through a midline laparotomy scar and two abdominal drains, with features of septicemic shock. He was operated on prior to admission at our institute for gangrenous small bowel. Pre-operative ECG was suggestive of atrial fibrillation, for which Amiodarone was given. After surgery, the patient developed an acute onset fistula and multiple intestinal perforations, which required re-exploration and extensive surgical repair. Conclusion: Acute mesenteric ischemia should be considered in cases of acute abdomen in elderly patients with cardiac illness presenting with abdominal pain. Prompt diagnosis and treatment should be initiated to ameliorate morbidity and mortality, and a re-look laparotomy must be considered in selected cases.
Keywords: Acute Mesenteric Ischemia, Intestinal Perforations, Anastomotic Dehiscence, Septic Shock
INTRODUCTION
Acute mesenteric ischemia is an uncommon but potentially fatal surgical emergency defined by an abrupt stoppage of blood supply to the intestines. If left untreated, this illness can cause severe mortality and morbidity due to inflammation and necrosis. Acute mesenteric ischemia has a complex aetiology, with the main contributors being trauma, atherosclerosis, thromboembolism, and aneurysms. Due to their increased risk of thromboembolic events, older people with pre-existing cardiac disorders, such as atrial fibrillation, are more likely to have acute mesenteric ischemia.
There are several difficulties in managing acute mesenteric ischemia, especially in individuals who have cardiac comorbidities. Patients with heart conditions are more likely to experience acute mesenteric ischemia as well as treatment-related consequences. An arrhythmia that is frequent in the elderly is atrial fibrillation, which raises the risk of thromboembolism and can obstruct mesenteric veins. Due to the ischemia and subsequent necrosis of the intestinal tissue resulting from intestinal obstruction, there is a surgical emergency that has to be managed immediately and aggressively.
Acute mesenteric ischemia presents challenging surgical treatment. Due to the non-specific presentation of symptoms, such as gastrointestinal discomfort and abdominal pain, which can be confused for other, less serious illnesses, the initial diagnosis is sometimes delayed. Accurate localisation and evaluation of the degree of ischemia and necrosis depend on imaging tests, such as contrast-enhanced CT scans.
In our case of a 53-year-old male patient, complications were aggravated by the development of several intestinal perforations following surgery. Acute Mesenteric Ischemia required meticulous treatment, which made the surgical and postoperative processes more difficult. The first surgical procedure included jejuno-colic anastomosis and gangrenous bowel resection. Re-examination shows the patient had septicemia and an abrupt onset gastrointestinal fistula. Extensive perforations near the jejunum's antimesenteric boundary are extremely uncommon and pose a major surgical risk.
This case study emphasises how crucial it is to diagnose patients as quickly as possible when immediate surgical intervention is required and how crucial complete post-operative care is for treating acute mesenteric ischemia in patients with cardiac comorbidities. Multiple perforations emphasise the severe and unpredictable nature of acute mesenteric ischemia, especially in a post-operative scenario. Surgical teams must be prepared to undertake complex repairs and re-exploration to decrease mortality and enhance patient outcomes.
CASE PRESENTATION
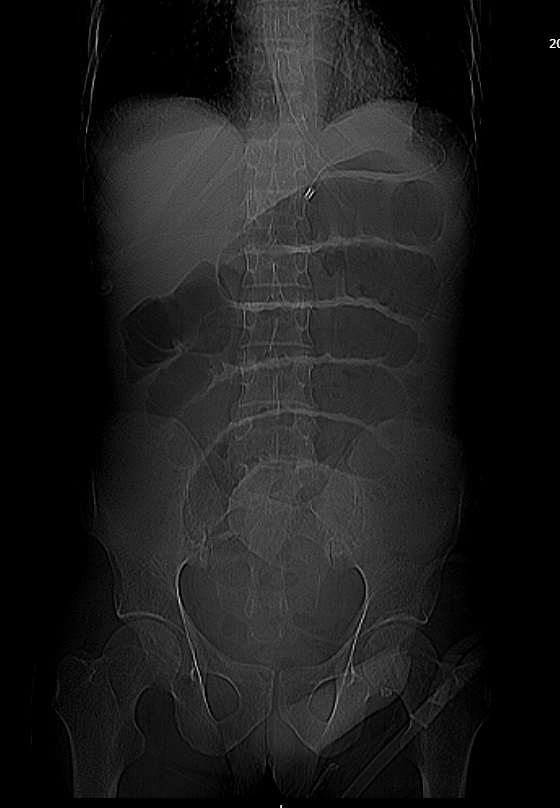
The 53-year-old male patient had a significant medical history, which included a recent small intestinal resection surgery for the gangrenous disease, and came to our tertiary care centre’s emergency department seven days after surgery, complaining of sudden, severe stomach discomfort, vomiting, and constipation. During the initial emergency visit at a private hospital, several dilated small intestinal loops suggestive of acute intestinal obstruction were seen on contrast-enhanced computed tomography (CECT) of the abdomen (Figure 1). Free air is also visible between bowel loops using CECT (Figure 2). He underwent resection of the small bowel, 30 cm from duodenojejunal flexure to 5 cm from ileocecal junction and closure of terminal ileum with end to side jejuno- colic anastomosis was done. Amiodarone was used to treat the patient's atrial fibrillation, which occurred after surgery. The patient was at risk for mesenteric ischemia due to a heart problem despite not having any history of previous thromboembolic episodes.
Figure 1. CECT Abdomen showing multiple dilated small intestinal loops.
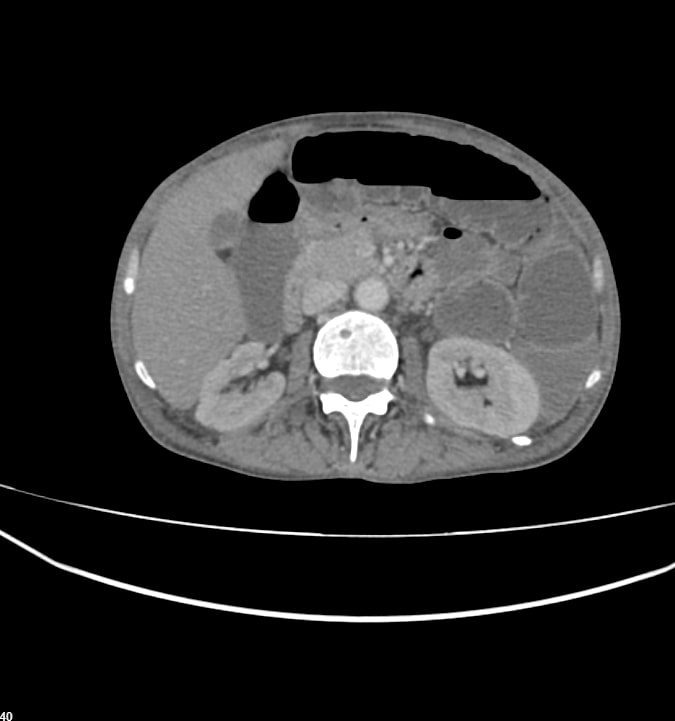 Figure 2. CECT showing free air between distended bowel loops.
Figure 2. CECT showing free air between distended bowel loops.
On local examination, the patient’s abdomen revealed midline purulent discharge with bilious staining, with two abdominal drains. The left drain tube consists of a purulent collection, and the right drain contains serous discharge. The patient had fever, hypotension, and tachycardia. The abdomen was distended on palpation, with guarding or rigidity and periumbilical tenderness, which suspects complex intra-abdominal pathology that was probably brought on by mesenteric ischemia and postsurgical complications.
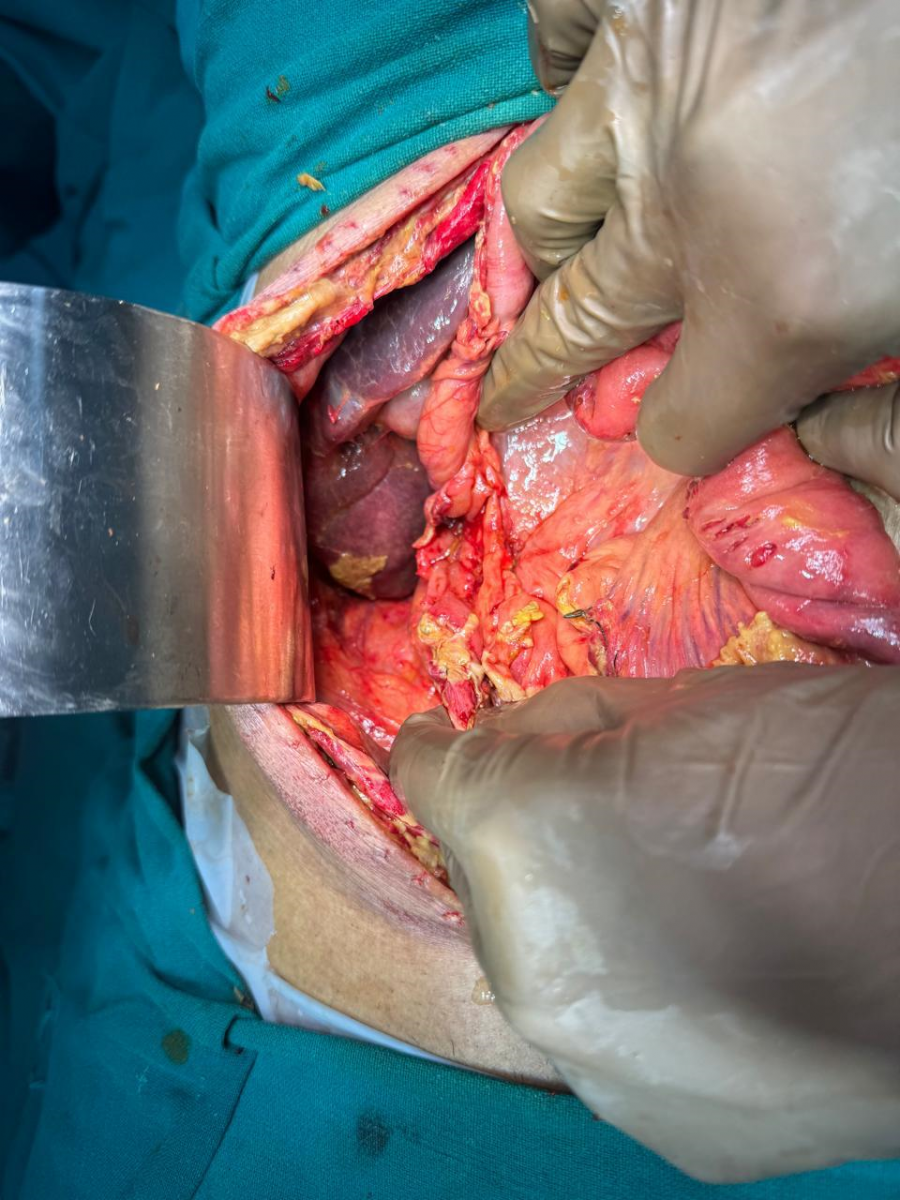
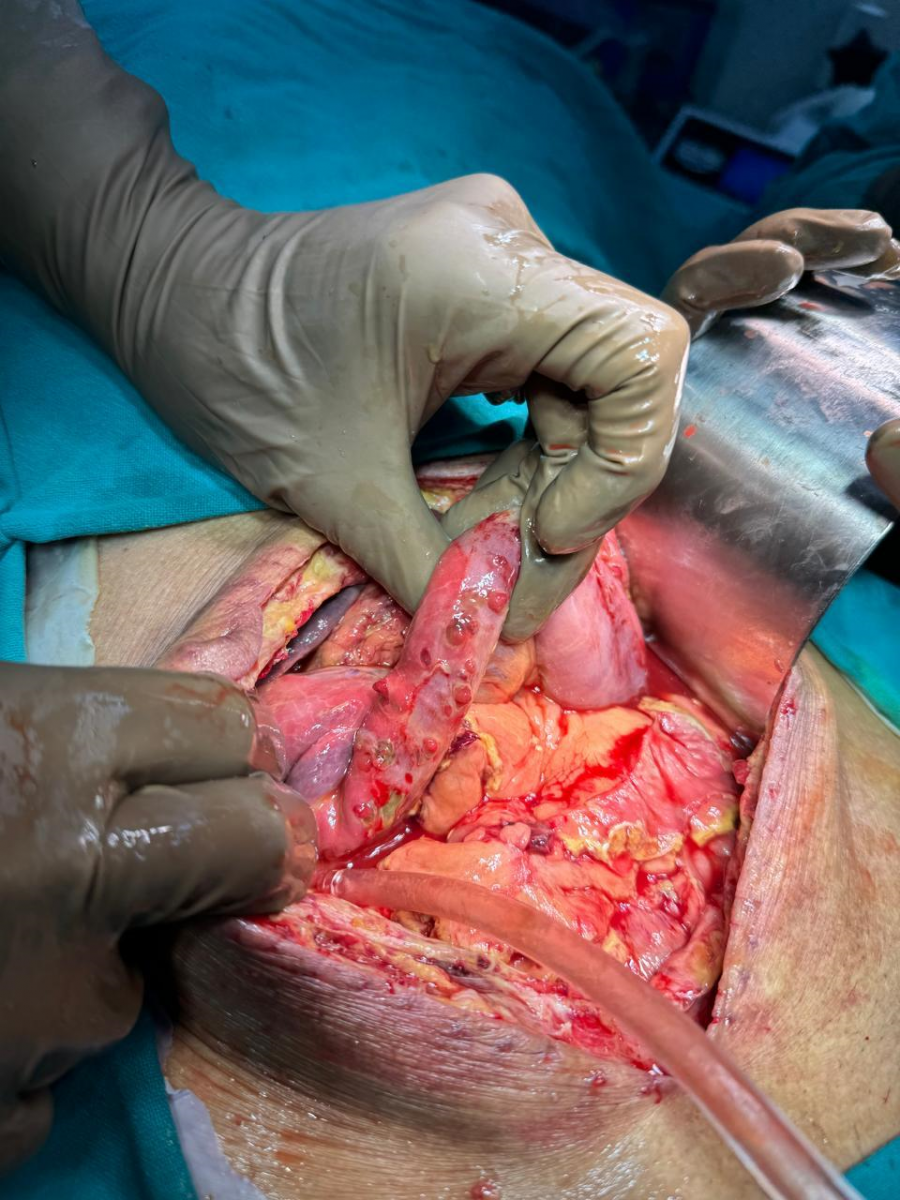
On the seventh postoperative day, a re-exploration laparotomy was conducted because of the patient's deteriorating health condition and the presence of signs of peritonitis. Anastomotic dehiscence at the jejuno-colic anastomosis and a notable leak from the ileal stump were noted intraoperatively (Figure 3). The most striking discovery was that the remaining jejunum's antimesenteric border had more than 60 intestinal perforations (Figure 4). These perforations were dispersed throughout the proximal jejunum and ranged in size. A colonic rent was discovered as well, and it was also repaired during the procedure. To prevent significant damage, the surgical team repaired the jejunal perforations and performed a jejunoileal anastomosis and an end duodenostomy.
Figure 3. Figure showing anastomotic dehiscence.
Figure 4. Figure showing multiple jejunal perforations.
After surgery, the patient was closely monitored for his hemodynamic condition and treated with broad-spectrum antibiotics in the intensive critical care unit. After receiving two-day treatment in the critical unit and antithrombotic prophylactic medications, the patient was successfully extubated. Due to the end duodenostomy and the risk of high output stoma, we started early total parenteral nutrition. The patient is planned for discharge after demonstrating improvement. He did, however, have atrial fibrillation once again while being admitted. The patient remained unstable despite aggressive supportive care. The patient's condition deteriorated, and he had acute respiratory distress syndrome (ARDS) and acute kidney failure following several days of intensive care. The patient succumbed to his condition due to severe consequences resulting from numerous intestinal perforations resulting from acute mesenteric ischemia.
DISCUSSION
Acute Mesenteric Ischemia is a serious illness that requires rapid diagnosis and treatment to prevent significant morbidity and death [1]. The consequences of acute mesenteric ischemia, particularly in individuals with cardiac comorbidities, poses significant challenges for surgical and medicinal management [2,3].
The presence of atrial fibrillation made managing acute mesenteric ischemia substantially more difficult. Atrial fibrillation raises the likelihood of thromboembolic events, which are the leading cause of mesenteric ischemia [2,4]. The use of amiodarone to treat arrhythmia, as well as the necessity for anticoagulant medication, increased the risk of complications during the perioperative period [5,6]. Managing these comorbidities while dealing with an emergent surgical emergency needed a precise balance to prevent worsening the patient's health [7,8].
Acute mesenteric ischemia requires prompt surgical care, especially when multiple intestinal perforations are present [3,9]. Our patient had a re-exploration of the abdomen done on the seventh postoperative day, which revealed anastomotic dehiscence, a leak from the ileal stump, and more than 60 perforations at the anti-mesenteric border of the remaining 30 cm jejunum. End Duodenostomy, with the repair of perforations, and jejunoileal anastomosis, with the repair of colonic rent, was performed. The first resection of gangrenous bowel, followed by jejuno-colic anastomosis and subsequent re-exploration to treat anastomotic dehiscence and numerous perforations, exemplifies the complexities of such procedures. Surgical choices, such as conducting an end duodenostomy and constructing a new anastomosis, were critical in attempting to control the extensive damage and infection.
Identification procedures for acute mesenteric ischemia can detect vascular occlusions and ischemic alterations in the gut, which can be done using imaging techniques such as contrast-enhanced CT scans [1]. Surgical revascularisation, intestinal resection, and supportive care are used to treat sepsis and multi-organ failure after the identification of mesenteric ischaemia [2]. Re-exploration and several surgical operations, along with antibiotic treatment, fluid resuscitation, and nutritional assistance, are all essential components of postoperative care after significant intestinal injury [3,5].
Patients with delayed diagnosis and comorbidities have a poor prognosis for acute mesenteric ischemia. Due to the rapid progression of intestinal necrosis and septic shock, acute mesenteric ischemia can cause death in 60 to 80% of cases [4,5]. The presence of multiple perforations and sepsis significantly diminishes the chances of survival when surgical intervention is delayed, as seen in our case. Early intervention and awareness regarding such difficult situations are essential for improving prognosis.
CONCLUSION
Acute mesenteric ischemia should be considered in older individuals with heart problems who arrive with acute abdomen. Early diagnosis and vigorous care, including re-look laparotomy, are critical for better results. This case further underlines the rarity and severity of multiple intestinal perforations in acute mesenteric ischemia, highlighting the need for surgical teams to be prepared for such acute surgical emergencies.
REFERENCES
- Clair DG, Beach JM. (2016). Mesenteric Ischemia. N Engl J Med. 374(15):1474-1479.
- Oldenburg WA, Lau LL, Rodenberg TJ, Edmonds HJ, Burger CD. (2004). Acute Mesenteric Ischemia: A Clinical Review. Arch Intern Med. 164(18):1054-1062.
- Karkos CD, Menexes GC, Patelis N, Bougioukas IG, Seretis C, Konstantinidis K, et al. (2017). Systematic Review and Meta-Analysis of the Prognostic Value of Inflammatory Markers in Acute Mesenteric Ischemia. Ann Vasc Surg. 41:129-140.
- Schoots IG, Koffeman GI, Legemate DA, Levi MM, van Gulik TM. (2004). Systematic Review of Survival After Acute Mesenteric Ischaemia According to Disease Aetiology. Br J Surg. 91(1):17-27.
- Montagnani S, Consolo F, Cestari R, Vazzana I, Di Marzo L, Barone G, et al. (2020). Acute Mesenteric Ischemia: Is It Time to Change the Paradigm? Ann Vasc Surg. 63:20-26.
- Tilsed JV, Casamassima A, Kurihara H, Mariani D, Martinez I, Pereira J, et al. (2016). ESTES guidelines: acute mesenteric ischaemia. Eur J Trauma Emerg Surg. 42(2):253-270.
- Oderich GS, Panneton JM, Hofer J, Bower TC, Cherry KJ, Sullivan TM, et al. (2009). Technical aspects and outcomes of endovascular therapy for acute mesenteric ischemia. J Vasc Surg. 49(4):698-704.
- Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, Gomes CA, et al. (2017). Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 12:38.
- Björck M, Wanhainen A. (2010). Nonocclusive mesenteric hypoperfusion syndromes: recognition and treatment. Semin Vasc Surg. 23(2):54-64.
 Abstract
Abstract  PDF
PDF